Today I respond to a reader’s request. She writes, “In my residency, we were told to give the patient the widest degree of decision-making and avoid making decisions for them. Sometimes this is hard to do because patients are unsure what to do even after I lay out the options in a lot of detail. I don’t want to be manipulative. Usually, I know how to work this out, but I would like to hear from you your approach to these kinds of dilemmas.”
Jack’s Response: There’s a lot lurking in this statement. The three goals are: 1) to optimize the patient’s autonomy, 2) to avoid “manipulating” the patient, and 3) to provide the patient with the treatment most likely to result in the best outcome.
Let me lay out four principles that I think can guide us to achieve the three goals stated above. They are fiduciary responsibility, standard of care, informed consent, and motivational enhancement.
Fiduciary Responsibility
As clinicians, we all have a legal and ethical responsibility to act in the patient’s best interests. This is the touchstone that separates influencing a patient to, on the one hand, make the best decision for themselves and have the motivation for implementing whatever strategies will help them achieve their goals and, on the other hand, influencing them to engage in activities that have other motives, such as making life easier on the clinician. The latter can occur when, for example, the patient insists on a treatment the clinician judges as being unlikely to help and/or likely to harm, yet provides that treatment anyway, like an abusable med, just to avoid having to tell the patient ‘No’.
When we influence a patient to choose something that is not in their best interest, we call that manipulation. Manipulation has both a neutral meaning – to influence, with the etymology being “to handle by hand” – and a negative meaning – to influence someone against their own best interests. So, influencing a patient is not necessarily a negative, but influencing them against their best interests is indeed a negative. I stress this because many clinicians conflate the two meanings and are hesitant to influence a patient. Influencing is not only acceptable but a core part of our jobs. Our patients, in their depression, anxiety, lack of focus, deficits of skill, and lack of motivation, need us to inspire them, to guide them, to help them make the best decision for themselves and then to carry through on it. That is a lot of influence we are called upon to exercise. We should do it ethically and well.
Standard of Care
Standard of care refers to the range of acceptable management options, that is, the options that an average clinician has the experience and knowledge to judge as having a reasonable chance of resolving the patient’s disease, disorder, or life problem with which they present. The more evidence the clinician can muster in support of their judgment, the stronger the case they can make to the patient – and in a courtroom, if it ever comes to that. The options that are offered to the patient all need to meet the standard of care. Those that do not should not be offered, and if requested by the patient, should be refused.
There is one exception: sometimes a clinician agrees to provide treatment which itself may not meet standard of care, but the clinician agrees to it in an effort and with a hope that the patient at a later point will be open to choosing a different and more adequate treatment. Thus, the clinician is striving towards provision of adequate treatment but doing so indirectly. Of course, if the clinician’s initial treatment clearly does not meet standard of care, the clinical notes need to reflect the clinician’s justification for doing so: that today’s inadequate treatment is in service of getting the patient to agree and adhere to adequate treatment at some foreseeable point in the future. This initial inadequate treatment should not be continued indefinitely, though. The clinician’s statements to the patient (and chart notes) should reflect that the clinician’s expectation and plan is to get the patient onto adequate treatment after some specific number of weeks, for example.
A patient’s initial refusal of adequate treatment can lead to an eventual change of heart for various reasons: the initial, inadequate treatment failed, and the patient is now ready to follow the clinician’s recommended treatment. Or the patient has gained enough trust in the clinician to allow themselves to follow that clinician’s recommendations despite their initial hesitation. Humans are unlikely to do what another person recommends if they do not trust that person’s competence or their motivation to do the right thing by them. Thus, the patient may need time to ‘assess’ or ‘test’ the clinician’s competence and caring. Once the clinician passes this ‘test’, the patient may then follow preferred treatment recommendations.
Informed Consent
When seeking to obtain informed consent, the clinician is obligated to provide the information necessary to allow the patient to make an informed decision, and to provide it at a level and pace appropriate to the patient’s ability to reason through it. Notice the prior sentence: it is not a straight shot from your provision of information to the patient’s informed decision-making. Rather, it is incumbent on you to set the conditions for successful patient information-understanding and decision-making. Sometimes this is accomplished quickly and sometimes slowly. You should provide the patient the opportunity to ask questions, and yourself the opportunity to assess the patient’s understanding. The reasons a patient may have difficulty or inability deciding can be due to attentional deficits, cognitive or educational deficits, or emotional or motivational impairment, among many others.
Motivational Enhancement
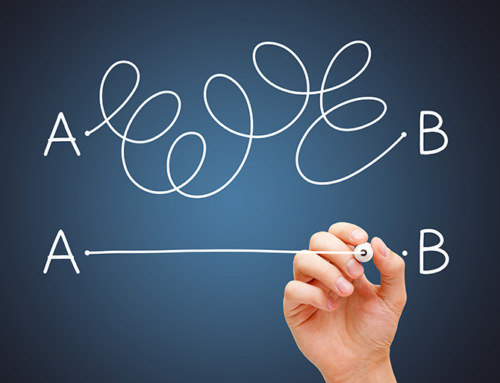
Today, I will not lay out the richness of motivational enhancement and save a detailed treatment of it for a future post. Instead, I’ll share my simple-minded way of thinking about it and presenting it to patients. It’s the “Point A – Point B” conceptualization, which has three main parts: Point A is the here and now, all the ways the patient is in pain, symptomatic, dysfunctional, facing a myriad of overwhelming problems, and feeling stuck. Point B is the desired outcome, a vision for what life would be like if the patient were able to move beyond their pain, symptoms, dysfunction, overwhelming problems, and stuckness. The third part consists of the barriers that impede moving from Point A to Point B.
To move through this approach, I say something like the following to the patient: “It sounds like you’re feeling frustrated and stuck. Our next step is to find the ways – practical and doable ones – to get you unstuck. The way I think about this is as the ‘Point A – Point B’ problem. You are now stuck at Point A, which you’ve described to me already. Point B is what you want in life and out of this treatment. So, let’s now focus on Point B, that is, describe to me in as much detail as possible what you want your life to be like if you could get unstuck”. Here I encourage the patient’s open-ended exploration of what their day-to-day activities would be like once they reach their desired state. In this exploration, I might throw in the ‘miracle question’ which is, “If you woke up tomorrow morning and all the problems you described to me were gone, like a miracle, what would your life be like? What would you be doing?”. It is important to force the patient to be specific by asking follow-up questions, such as, “What time would you get up each morning? What would you eat for breakfast? What would you do to improve your finances? What would your relationship with your kids be like? What would you do for fun? How would you handle new problems as they arise because, we can be sure, new problems will arise?”. The goal is to have the patient visualize and feel their future life, to have a rich imaginal experience of it. During this exercise, some patients realize they never really thought about what their alternative better life would/could be like. They had always focused on their pain, symptoms, dysfunction, forgetting that the amelioration of the bad stuff does not directly translate into a life worth living. A compelling positive vision of what life can be like is often a necessary ingredient in moving forward.
The last step of this model is exploring and fixing the barriers to moving from Point A to Point B. Note that barriers include both bad things that exist in the person’s life and good things that are absent. A violent domestic partner may be a bad thing that is in place, while childcare support may be a good thing that is absent. As with the previous parts of the model, the barriers – what needs to be removed or overcome and what needs to be added – need to be explored in detail. The rubber needs to hit the road. The patient must be guided to consider, choose, and carry out practical and doable solutions. There are likely many problems that need resolving and likely many changes to be made. The patient should be guided to prioritizing and choosing the first step. My approach is to say, “It’s not uncommon to get a little overwhelmed when thinking about all these changes that need making. The best way to succeed is to choose one thing to change and start there. And then, over time, add other things to change. So, in your judgment, what is the single thing you believe would make the biggest difference in your life right now?”.
If all this sounds like a lot of work that will take a lot of time, it usually is exactly that. The alternative is like what much of psychotherapy is actually like, an endless focus on the problems, frustration, stuckness, etc., without adequate focus on moving through solutions into a desired life. For example, many people in treatment for an addiction would like to stay clean and sober. But staying clean and sober requires many concrete choices and actions carried out over extended periods of time. Often the motivation for change is low and not robust in the face of setbacks, not because the current life of active addiction is great, but rather because the life of sober living seems unattainable and perhaps not even that compelling. Exploring in detail Point B as well as the barriers that need addressing can help increase motivation, hope, and a feeling of growing agency.
To end, the reason I riffed on motivational enhancement is that it is my way of responding to fears of manipulating the patient. Do I manipulate the patient by increasing their motivation, trying to get them to think about things they haven’t thought about, and to take actions they otherwise might not undertake? Of course I do. The better I can do this, the more effective I become.
I already mentioned that negative manipulation occurs when I guide the patient toward goals that are not in their best interests. But there is an additional, more subtle point to make: the line between motivation enhancement and less-than-good manipulation is the latter occurs when I, rather than taking the time to explore the patient’s Point B, assume it and guide the patient towards my assumption. In this case, I’m not guiding the patient against their best interests, but rather assuming I know what the patient’s best interests are. Maybe this isn’t negative manipulation, but it is using one’s power to influence in a way that could lead to outcomes that are less than they otherwise could be.
Thanks for reading and take care,
Dr. Jack
LanguageBrief
“I am so tired – so tired of being of being whirled on through all these phases of my life, in which nothing abides by me, no creature, no place; it is like the circle in which the victims of earthly passion eddy continually.” ― Elizabeth Gaskell
“This I choose to do. If there is a price, this I choose to pay. If it is my death, then I choose to die. Where this takes me, there I choose to go. I choose. This I choose to do.” ― Terry Pratchett
“To be a person is to be constantly engaged in making yourself into that person” ― Christine M. Korsgaard
“One day, in retrospect, the years of struggle will strike you as the most beautiful.” ― Sigmund Freud
“Storytelling reveals meaning without committing the error of defining it.” ― Hannah Arendt
“To be rooted is perhaps the most important and least recognized need of the human soul.” ― Simone Weil






Leave A Comment